Venous thrombosis
Normal anatomy
|
|
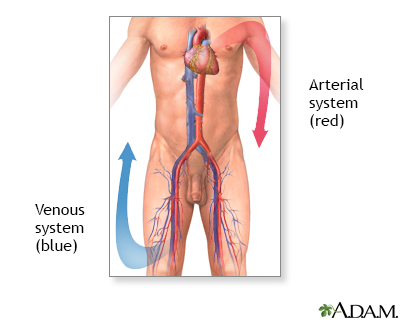
Veins carry blood back to the heart from the tissues. Blood flowing in the veins is under lower pressure and moves more slowly than blood flowing in the arteries. Blood is therefore more likely to clot in the veins, thus blocking the flow through the veins.
|
Indications
|
|
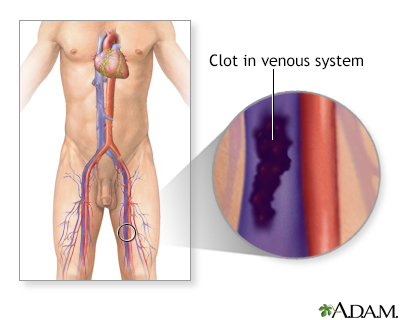
Blood clot formation in the veins is called venous thrombosis. Venous thrombosis most commonly forms in the veins of the legs. Risk factors for venous thrombosis include prolonged bed rest or immobility, as can be necessary after surgery, cancer, and estrogen therapy.
|
Procedure, part 1
|
|
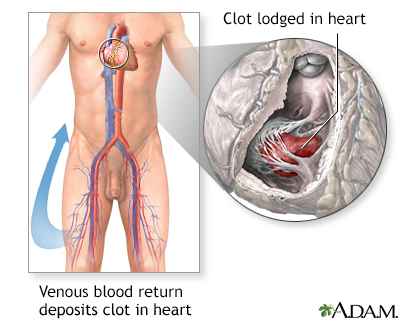
Venous thrombosis can cause swelling and pain of the leg in which it forms. Large clots can also break free and travel to the heart and lungs, where they can cause cardiac arrest and sometimes death. This is called pulmonary embolism.
|
Procedure, part 2
|
|
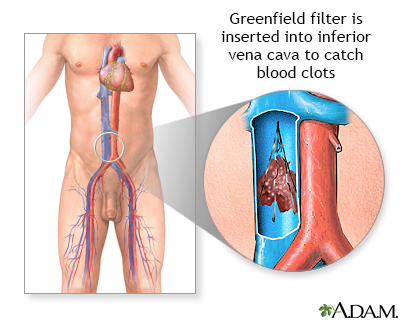
Venous thrombosis of the legs is diagnosed by ultrasound. Treatment usually involves medication to thin the blood and dissolve the thrombosis. Two common medications are heparin and coumadin.
If patients are not candidates for blood-thinning medication (such as patients with a history of stroke or bleeding), a filter is placed in the large vein leading from the leg to the heart, to catch any clot that may embolize up toward the heart. These filters can be inserted through a catheter inserted in the veins of the groin.
|
Aftercare
|
|
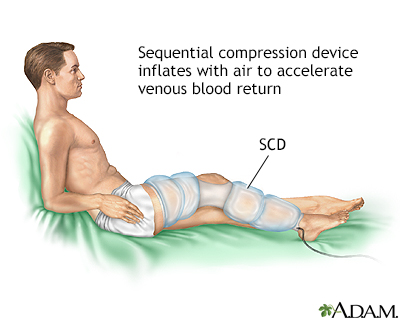
Post-operative patients are at risk for pulmonary embolism because of the time spent in bed after surgery. One method for reducing the risk of venous thrombosis is the use of sequential compression devices (SCDs). These are stockings that wrap around the legs and periodically inflate and deflate with air.
In part, this prevents the formation of thrombosis in the leg veins by increasing blood flow through the veins. The use of SCDs and early ambulation after surgery greatly reduces the risk of venous thrombosis and pulmonary embolism. Walking immediately after surgery also reduces the risk of thrombosis and pulmonary embolism.
SCDs are used after many major surgeries until patients are able to walk regularly on their own.
|

Review Date:4/18/2023
Reviewed By:John Roberts, MD, Professor of Internal Medicine (Medical Oncology), Yale Cancer Center, New Haven, CT. He is board certified in Internal Medicine, Medical Oncology, Pediatrics, Hospice and Palliative Medicine. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
The information provided herein should not be used during any medical emergency
or for the diagnosis or treatment of any medical condition. A licensed medical professional
should be consulted for diagnosis and treatment of any and all medical conditions. Call 911
for all medical emergencies. Links to other sites are provided for information only -- they
do not constitute endorsements of those other sites. © 1997-A.D.A.M., Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
The Agency for Health Care Administration (Agency) and this website do not claim the information on, or referred to by, this site is error free. This site may include links to websites of other government agencies or private groups. Our Agency and this website do not control such sites and are not responsible for their content. Reference to or links to any other group, product, service, or information does not mean our Agency or this website approves of that group, product, service, or information.
Additionally, while health information provided through this website may be a valuable resource for the public, it is not designed to offer medical advice. Talk with your doctor about medical care questions you may have.