Coronary artery balloon angioplasty
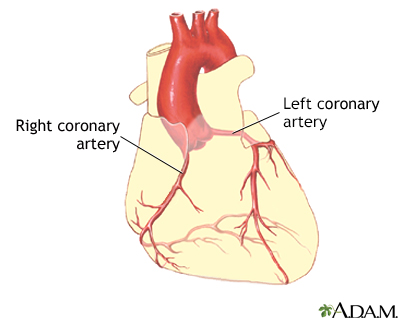
Normal anatomy
|
|
The coronary arteries supply blood to the heart muscle. The right coronary artery supplies both the left and the right heart; the left coronary artery supplies the left heart.
|
Indication
|
|
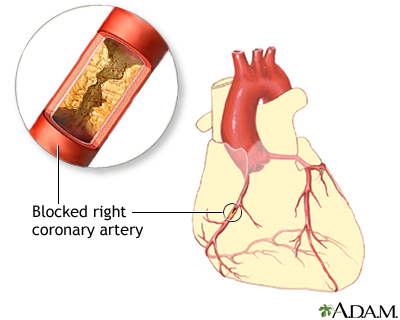
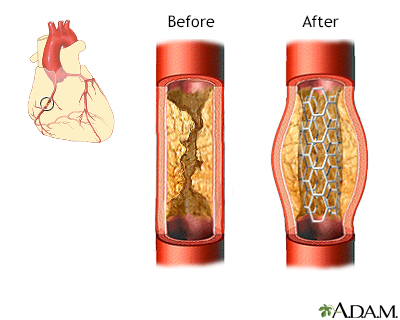
Fat and cholesterol accumulates on the inside of arteries (atherosclerosis). The small arteries of the heart muscle (the coronary arteries) can be narrowed or blocked by this accumulation. If the narrowing is small, percutaneous transluminal coronary angioplasty, or PTCA for short, may be the course for treatment. PTCA is a minimally invasive procedure to open up blocked coronary arteries, allowing blood to circulate unobstructed to the heart muscle. The indications for PTCA are:
- Persistent chest pain (angina)
- Blockage of only one or two coronary arteries
|
Procedure, part 1
|
|
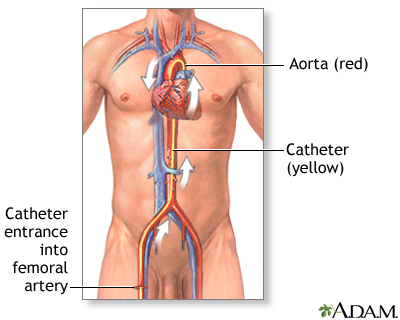
While the patient is awake and pain-free (local anesthesia), a catheter is inserted into an artery at the top of the leg (the femoral artery). The procedure begins with the doctor injecting some local anesthesia into the groin area and putting a needle into the femoral artery (the blood vessel that runs from the heart down the leg). Once the needle is inserted, a guide wire is placed through the needle, into the blood vessel. Following this step, the guide wire is left in the blood vessel and the needle is removed. A large needle called an introducer is then placed over the guide wire and the guide wire is removed.
|
Procedure, part 2
|
|
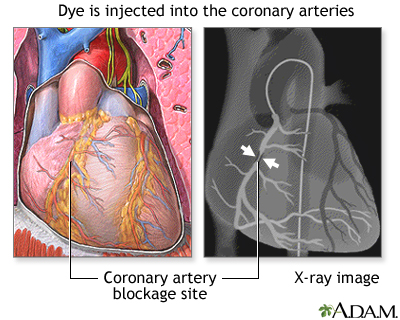
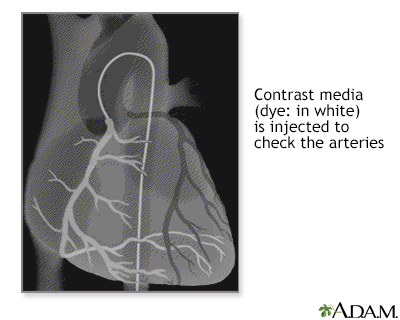
Next, a diagnostic catheter, which is a long narrow tube, is advanced through the introducer over a .035 inch (.0889 cm) guidewire, into the blood vessel. This catheter is then guided to the aorta and the guidewire is removed. Once the catheter is placed in the opening or ostium of one of the coronary arteries, the doctor injects dye and takes a series of X-rays (film of the images).
|
Procedure, part 3
|
|
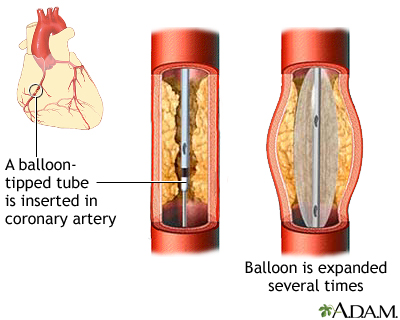
The first catheter is exchanged out over the guidewire for a guiding catheter and the guidewire is removed. A smaller guidewire is advanced across the blocked section of the coronary artery and a balloon-tipped tube is positioned so the balloon part of the tube is beside the blockage. The balloon is then inflated for a few seconds to compress the blockage against the artery wall. Then the balloon is deflated. The doctor may repeat this a few times, each time pumping up the balloon a little more to widen the passage for the blood to flow through. This treatment may be repeated at each blocked site in the coronary arteries.
|
Procedure, part 4
|
|
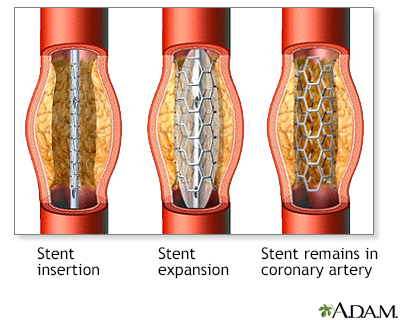
A device called a stent may be placed. A stent is a latticed, metal scaffold that is placed within the coronary artery to keep the vessel open.
|
Procedure, part 5
|
|
Once the catheter has been positioned at the coronary artery origin, contrast media is injected and a series of X-rays (film) are taken to check for any change in the arteries. Following this, the catheter is removed and the procedure is completed.
|
Aftercare, part 1
|
|
This procedure can greatly improve the blood flow through the coronary arteries and to the heart tissue in about 90% of patients and may eliminate the need for coronary artery bypass surgery. The outcome is relief from chest pain symptoms and an improved exercise capacity. In 2 out of 3 cases, the procedure is considered successful with complete elimination of the narrowing or blockage.
This procedure treats the condition but does not eliminate the cause and recurrences happen in 1 out of 3 to 5 cases. Patients should consider diet, exercise, and stress reduction measures. If adequate widening of the narrowing is not accomplished, heart surgery (coronary artery bypass graft surgery, also called a CABG) may be recommended.
|
Aftercare, part 2
|
|
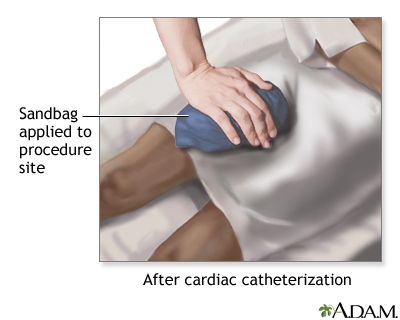
Immediately after the procedure, a ten-pound (5 kg) sandbag may be placed over the femoral artery puncture site in the leg and remain there for 6 hours. This is done to help the artery heal.
|

Review Date:1/1/2023
Reviewed By:Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
The information provided herein should not be used during any medical emergency
or for the diagnosis or treatment of any medical condition. A licensed medical professional
should be consulted for diagnosis and treatment of any and all medical conditions. Call 911
for all medical emergencies. Links to other sites are provided for information only -- they
do not constitute endorsements of those other sites. © 1997-A.D.A.M., Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
The Agency for Health Care Administration (Agency) and this website do not claim the information on, or referred to by, this site is error free. This site may include links to websites of other government agencies or private groups. Our Agency and this website do not control such sites and are not responsible for their content. Reference to or links to any other group, product, service, or information does not mean our Agency or this website approves of that group, product, service, or information.
Additionally, while health information provided through this website may be a valuable resource for the public, it is not designed to offer medical advice. Talk with your doctor about medical care questions you may have.