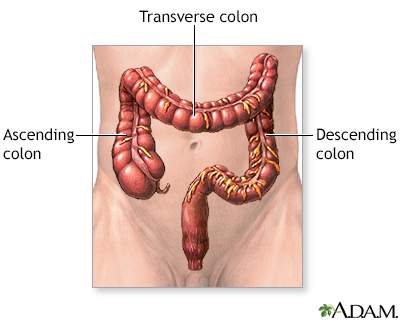
Large bowel resection
Normal anatomy
|
|
The large bowel [large intestine or the colon] is part of the digestive system. It runs from the small intestine to the rectum. It is made up of three portions; the ascending, transverse and descending colon. The ascending colon is sometimes referred to as the right colon; the descending colon is sometimes referred to as the left, or sigmoid colon.
|
Indications
|
|
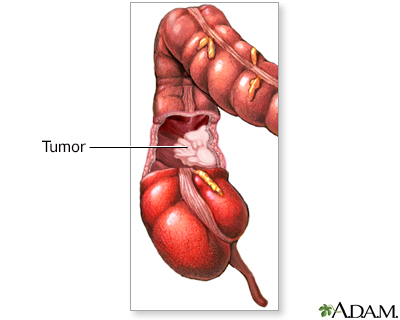
Bowel resection may be indicated for:
- Blockage of the intestine (intestinal obstruction) due to scar tissue or tumors
- Bleeding, due to diverticulosis or arteriovenous malformations
- Injuries
- Cancer
- Precancerous polyps
- Familial polyposis
- Infection, due to diverticulitis
|
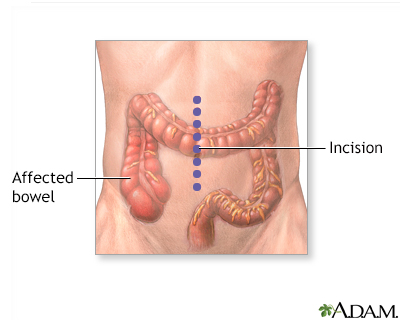
Incision
|
|
The patient is deep asleep and pain-free (general anesthesia). A lower midline incision is made in the abdomen. Sometimes, the surgeon will use a lateral lower transverse incision instead.
|
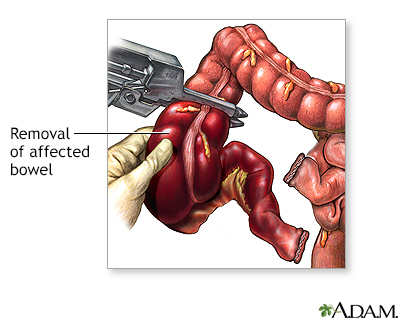
Procedure, part 1
|
|
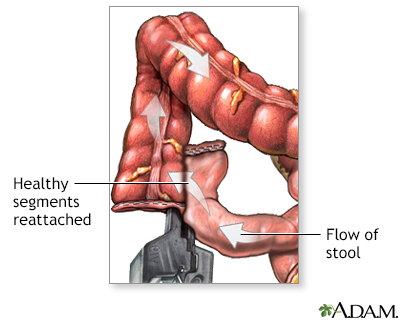
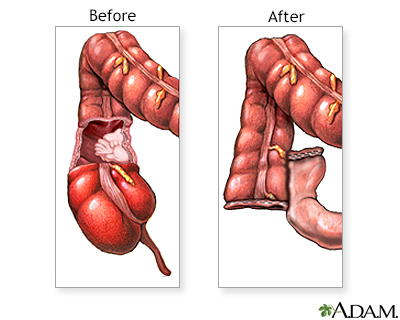
The diseased part of the large intestine (colon) is removed. The two healthy ends are then sewn or stapled back together and the incision is closed. A stapling procedure is shown here.
|
Procedure, part 2
|
|
If it is necessary to spare the intestine from its normal digestive work while it heals, a temporary opening of the intestine onto the abdomen (colostomy) may be done. A temporary colostomy will be closed and repaired later. If a large portion of the bowel is removed, the colostomy may be permanent. The large intestine (colon) absorbs most of the fluid from foods. When the colon is bypassed by a colostomy in the right colon, the colostomy output is generally liquid stool (feces). If the colon is bypassed in the left colon, the colostomy output is generally more solid stool. The constant or frequent drainage of liquid stool can cause the skin around the colostomy to become inflamed. Careful skin care and a well-fitting colostomy bag can reduce this irritation.
|
Aftercare
|
|
Most patients will stay in the hospital for 5 to 7 days. Complete recovery from surgery may take 2 months. During the first few days after surgery, eating is restricted.
|

Review Date:4/18/2023
Reviewed By:John Roberts, MD, Professor of Internal Medicine (Medical Oncology), Yale Cancer Center, New Haven, CT. He is board certified in Internal Medicine, Medical Oncology, Pediatrics, Hospice and Palliative Medicine. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
The information provided herein should not be used during any medical emergency
or for the diagnosis or treatment of any medical condition. A licensed medical professional
should be consulted for diagnosis and treatment of any and all medical conditions. Call 911
for all medical emergencies. Links to other sites are provided for information only -- they
do not constitute endorsements of those other sites. © 1997-A.D.A.M., Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
The Agency for Health Care Administration (Agency) and this website do not claim the information on, or referred to by, this site is error free. This site may include links to websites of other government agencies or private groups. Our Agency and this website do not control such sites and are not responsible for their content. Reference to or links to any other group, product, service, or information does not mean our Agency or this website approves of that group, product, service, or information.
Additionally, while health information provided through this website may be a valuable resource for the public, it is not designed to offer medical advice. Talk with your doctor about medical care questions you may have.