Omphalocele repair
Normal anatomy
|
|
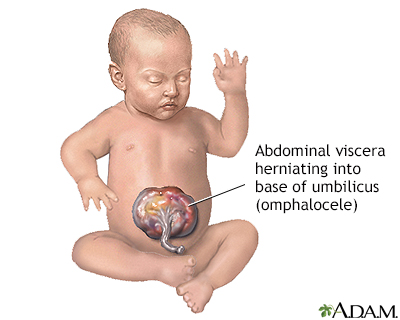
Omphalocele is an abdominal wall defect at the base of the umbilical cord (umbilicus); the infant is born with a sac protruding through the defect which contains small intestine, liver, and large intestine. Omphalocele is frequently associated with other birth defects, such as heart defects, imperforate anus, urinary problems, and genetic defects. Omphalocele is very similar to gastroschisis, except that the organs are enclosed in a sac.
|
Indications
|
|
Omphalocele is a life-threatening event requiring immediate intervention. The infant may be born underweight (small for gestational age) due to stress from this condition before birth.
|
Procedure
|
|
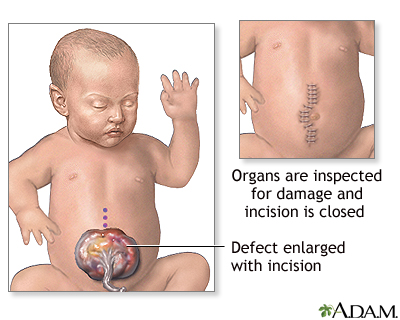
Immediately after delivery, the exposed organs are covered with warm, moist, sterile dressings. A tube is inserted into the stomach (nasogastric tube, also called NG tube) to keep the stomach empty to prevent choking on or breathing in (aspiration) stomach contents into the lungs. The surgery is done as soon as the infant is stable.
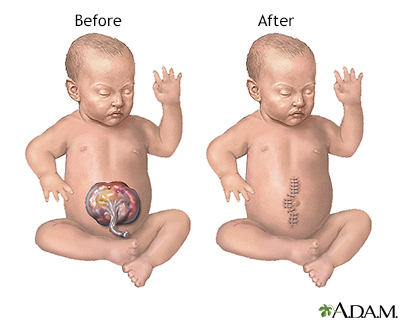
While the baby is deep asleep and pain-free (under general anesthesia) an incision is made to remove the sac membrane. The bowel is examined closely for signs of damage or additional birth defects. Damaged or defective portions are removed and the healthy edges stitched together. A tube is inserted into the stomach (gastrostomy tube) and out through the skin. The organs are replaced into the abdominal cavity and the incision closed, if possible.
|
Aftercare
|
|
The infant is cared for post-operatively in a neonatal intensive care unit. The baby is placed in an isolette (incubator) to keep warm and prevent infection. Oxygen is given and mechanical ventilation is often required. Intravenous fluids, antibiotics, and pain medications will be given. A nasogastric tube will be in place to keep the stomach emptied of gastric secretions. Feedings are started by nasogastric tube as soon as bowel function resumes. Feedings are started very slowly and often infants are reluctant to feed. These babies may need feeding therapy and lots of encouragement.
|

Review Date:3/11/2023
Reviewed By:Debra G. Wechter, MD, FACS, General Surgery Practice Specializing in Breast Cancer, Virginia Mason Medical Center, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
The information provided herein should not be used during any medical emergency
or for the diagnosis or treatment of any medical condition. A licensed medical professional
should be consulted for diagnosis and treatment of any and all medical conditions. Call 911
for all medical emergencies. Links to other sites are provided for information only -- they
do not constitute endorsements of those other sites. © 1997-A.D.A.M., Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
The Agency for Health Care Administration (Agency) and this website do not claim the information on, or referred to by, this site is error free. This site may include links to websites of other government agencies or private groups. Our Agency and this website do not control such sites and are not responsible for their content. Reference to or links to any other group, product, service, or information does not mean our Agency or this website approves of that group, product, service, or information.
Additionally, while health information provided through this website may be a valuable resource for the public, it is not designed to offer medical advice. Talk with your doctor about medical care questions you may have.