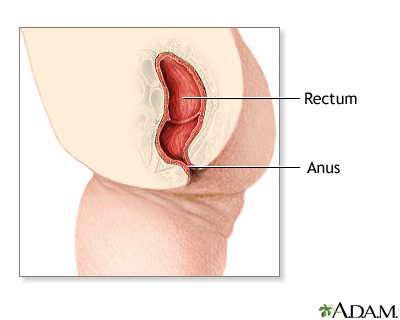
Imperforate anus repair
Normal anatomy
|
|
In individuals with a normal anatomy, the large intestine (colon) empties into a pouch-like portion of bowel (rectum). Through complex nerve and muscle structures, the rectum releases stool through the anus out of the body.
|
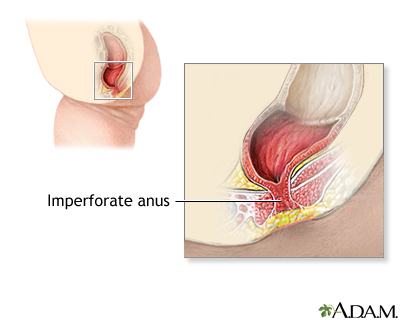
Indications
|
|
This surgery is recommended to repair cases of imperforate anus and other anorectal malformations. There are two types of imperforate anus; a low type and a high type. The low type imperforate anus repair is illustrated.
|
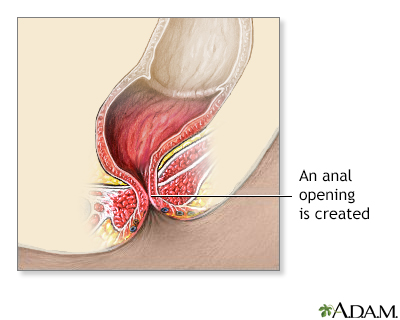
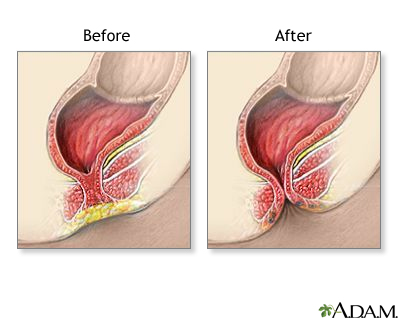
Procedure
|
|
Surgical repair involves creating an opening for passage of stool. Complete absence of an anal opening requires emergency surgery for the newborn.
Surgical repairs are done while the baby is deep asleep and pain-free (using general anesthesia).
Surgery for a high type imperforate anus defect usually involves creation of a temporary opening of the large intestine (colon) onto the abdomen to allow passage of stool (this is called a colostomy). The baby is allowed to grow for several months before attempting the more complex anal repair.
The anal repair involves an abdominal incision, loosening the colon from its attachments in the abdomen to allow it to be repositioned. Through an anal incision, the rectal pouch is pulled down into place, and the anal opening is completed. The colostomy may be closed during this stage or may be left in place for a few more months and closed at a later stage.
Surgery for the low type imperforate anus (which frequently includes a fistula) involves closure of the fistula, creation of an anal opening, and repositioning the rectal pouch into the anal opening.
A major challenge for either type of defect and repair is finding, using, or creating adequate nerve and muscle structures around the rectum and anus to provide the child with the capacity for bowel control.
|
Aftercare
|
|
The child may require several days in the hospital. Dilatation of the new anus (to improve muscle tone and prevent narrowing) will begin in the hospital and continue for some months. Stool softeners and a high-residue diet will need to continue throughout childhood.
|

Review Date:9/9/2023
Reviewed By:Debra G. Wechter, MD, FACS, General Surgery Practice Specializing in Breast Cancer, Virginia Mason Medical Center, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
The information provided herein should not be used during any medical emergency
or for the diagnosis or treatment of any medical condition. A licensed medical professional
should be consulted for diagnosis and treatment of any and all medical conditions. Call 911
for all medical emergencies. Links to other sites are provided for information only -- they
do not constitute endorsements of those other sites. © 1997-A.D.A.M., Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
The Agency for Health Care Administration (Agency) and this website do not claim the information on, or referred to by, this site is error free. This site may include links to websites of other government agencies or private groups. Our Agency and this website do not control such sites and are not responsible for their content. Reference to or links to any other group, product, service, or information does not mean our Agency or this website approves of that group, product, service, or information.
Additionally, while health information provided through this website may be a valuable resource for the public, it is not designed to offer medical advice. Talk with your doctor about medical care questions you may have.